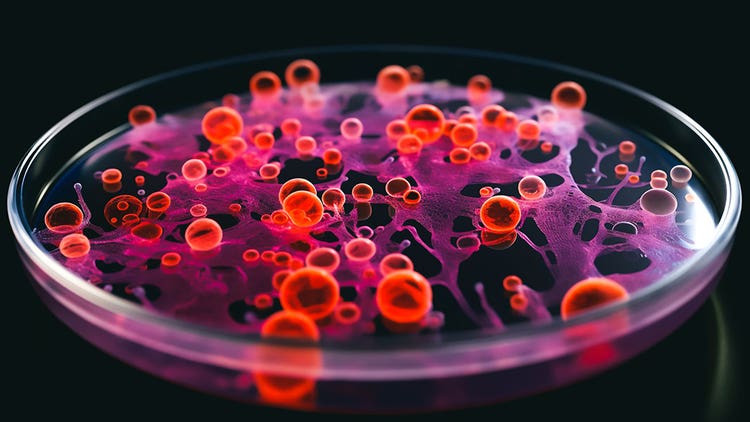
What Are Organoids?
Organoids are cellular structures grown in vitro to mimic the three-dimensional (3D) architecture of complex tissue and organ structures. Organoids can be developed from stem cells, cell lines, cancer cells and primary cells. Research with organoids has shown great promise in disease modeling, regenerative medicine, drug discovery and development. Additionally, because organoids can be created from a patient’s own cells, they offer a unique opportunity to enable personalized medicine.

Organoid and Related In Vitro Models
Organoids, spheroids and organ-on-a-chip models are all in vitro models that can be used to study human organs or tissues, but they differ in terms of their complexity, cellular diversity and physiological relevance. Organoids are the most complex and physiologically relevant, followed by organ-on-a-chip models, while spheroids are the simplest and commonly used for drug screening assays.
There are some key differences between these models:
Organoids: Organoids are 3D structures derived from stem cells or tissue explants and are capable of self-organizing to form functional tissue structures. Organoids can recapitulate the complex architecture and cellular heterogeneity of human organs, making them a valuable tool for disease modeling and drug screening. They can be cultured in vitro for extended periods, providing an opportunity to study long-term tissue dynamics and cellular interactions.
Organ-on-a-chip: Organ-on-a-chip is a microfluidic platform that allows for the growth and maintenance of miniature 3D organ-like structures in a controlled environment. Organ-on-a-chip models are designed to mimic the physiological and mechanical properties of human organs, such as the lung, liver, or heart, by recreating the organ's microenvironment and cellular interactions. Organ-on-a-chip models are being used to study the effects of drugs and toxins on specific organs and test the efficacy of new therapies.
Spheroids: Spheroids are 3D cell clusters that can be generated from various cell types, including cancer cells, stem cells and primary cells. They do not have the complex architecture and cellular diversity of organoids, nor are they exposed to the mechanical properties like organ-on-a-chip. Spheroids are typically used as simplified models of tissues or organs and are often employed in drug screening assays.
Establishment of 3D Spatial Organization
Organoids can be generated by using a variety of methods, including but not limited to:
Seeding on an Extracellular Matrix Scaffold - The extracellular matrix is the non-cellular material that surrounds and supports cells. It helps to maintain cell shape, anchor cells to one another and provide a surface for cell migration and signaling.
Cellular 3D Printing - This method utilizes a mixture of cells and scaffolding to precisely pattern cells analogous to the native organ or tissue. The organoids are first designed in silico to precisely draft each cell’s positioning then ‘printed’ into the culture system before adding cell culture media.
Patterning with Cell Adhesion Molecules - Cell adhesion molecules are proteins that mediate interactions between cells. Depending on their specific function, they can be used to promote or inhibit cell-cell adhesion.
Applying Mechanical Forces - Mechanical forces can be used to influence the formation of organoids. Stretching of cells or application of fluid forces can influence the maturation and/or migration of cells to help build desired architecture.
Organoid Model Systems
The development of novel organoid applications, including miniaturized models, has opened up exciting new avenues for biomedical research. These in vitro models provide an opportunity to study human organs and tissues in a more physiologically relevant context, allowing for a better understanding of disease mechanisms and the development of new therapies. Cerebral organoids have the potential to revolutionize our understanding of brain development and neurodegenerative diseases, while gut and stomach organoids can be used to study gastrointestinal diseases and test the efficacy of new therapies. Kidney organoids can help researchers better understand renal development and disease, and cancer organoids (tumoroids) can be used to study cancer biology and drug resistance and test personalized medicine approaches. Organoid applications have the potential to advance our understanding of human physiology and disease and to accelerate the development of new treatments.
Cerebral Organoid
A cerebral organoid is a miniaturized brain-like structure that can be used to study the development and function of the human brain and to model neurological diseases. These structures display basic features of neuronal activity, such as spontaneous electrical activity and the formation of synapses between neurons.
Gut Organoid
A gut organoid models the human gastrointestinal tract (GIT) and are being used to study its development and function to test new drugs and therapies for disease such as inflammatory bowel disease (IBD), celiac disease and irritable bowel syndrome (IBS). The process of creating a gut organoid can take weeks to form and resemble small pieces of intestine. They can contain all the major cell types in the GIT, including enterocytes, goblet cells, Paneth cells, enteroendocrine cells, smooth muscle cells and stromal cells.
Stomach or Gastric Organoid
The stomach is a muscular, J-shaped organ in the digestive system. It has three main functions: storing food, breaking down food and secreting digestive enzymes. The gastric organoid can replicate the stomach architecture and exhibit some or all these functions. It represents a novel way to study the stomach in vitro by providing a physiologically relevant model vs a two-dimensional cell culture model. Additionally, the gastric organoid can be used to study other aspects of gastrointestinal physiology, such as motility and acid secretion.
Kidney Organoids
The biogenesis of kidney organoids presents an attractive platform for drug discovery because they can be used to model both normal kidney function and disease. Kidney organoids have been used to study renal cystic diseases such as autosomal dominant polycystic kidney disease (ADPKD).
Organoids in Cancer Research
Organoids are increasingly being used in cancer research as models for studying disease and testing potential treatments. Organoids derived from patient tumor cells are commonly referred to as tumoroids and are matched to a control grown from healthy tissue or cells. Tumoroids are used for drug screening or to understand how cancer cells metastasize and to identify new biomarkers.
Tumoroids can be generated from both primary patient samples and established cancer cell lines. Foreskin or bladder epithelium can be used to generate urothelial carcinoma (UCC) tumoroids, while pancreatic adenocarcinoma (PDAC) tumoroids can be generated from pancreatic ductal epithelial cells.
One advantage of using organoids in cancer research is that they can be generated from a patient’s own tumor tissue, which allows for a personalized medicine approach.
Organoids and Personalized Medicine
Organoids have great potential for personalized medicine, as they can be generated from a patient's own cells and recapitulate the cellular heterogeneity and while maintaining the genetic makeup of the patient's organ or tumor. This approach allows for the creation of in vitro platforms for personalized drug screening and testing. Tumoroids generated from a patient biopsy can be used to screen a panel of drugs to identify the most effective treatment for that patient. This approach can also be used to test the efficacy and toxicity of new drugs on patient specific organoids reducing the time and cost of drug development. In addition, patient-derived organoids can be used to study disease mechanisms and to identify genetic mutations or biomarkers associated with a particular disease, which can inform personalized treatment decisions.
Organoids and in Vivo Studies
Organoids have the potential to replace some in vivo studies by providing a physiologically relevant in vitro model that can recapitulate the complex architecture and cellular diversity of human organs or tumors. This approach offers several advantages over traditional in vivo studies, such as reduced costs, time and risk of failure attributed to differences in biology and physiology of animal models.
Furthermore, organoids can be used to model genetic diseases, such as cystic fibrosis, by incorporating patient-specific mutations into the organoid culture. This approach can provide a platform for testing the efficacy of new drugs or gene therapies before they are tested in vivo.
However, it is important to note that organoids have some limitations and cannot fully replace in vivo studies. Organoids lack the complex tissue interactions and physiological responses and may not fully represent the complexity of the whole organism.
Applications of Organoids
The future applications of organoids have the potential to improve biomedical research and clinical practice. Some potential current and future applications of organoids include:
Tissue Engineering: Organoids can be used to engineer functional tissues and organs for transplantation. This approach has the potential to overcome the shortage of donor organs and provide personalized tissues and organs that are immunocompatible with the patient.
Neuroscience: Organoids can be used to study the development of the nervous system, model neurodegenerative diseases and develop new treatments for neurological disorders.
Disease Modeling: Organoids will increasingly be used to model various diseases, including genetic disorders, infectious diseases and cancer. This can help researchers better understand disease mechanisms and develop new treatments.
As technology continues to advance, organoids will likely become even more complex and versatile, providing an even more powerful tool for research and therapy.
See how Danaher Life Sciences can help
Organoids