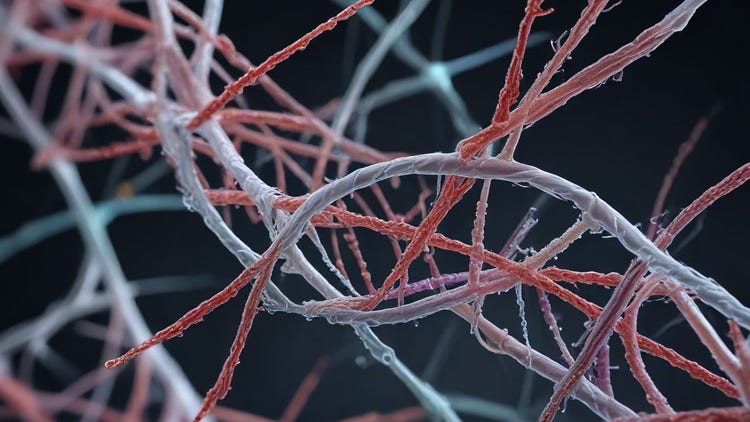
The essential biological processes in the body are not only governed by our cells. A complex web of macromolecules called the extracellular matrix (ECM) exists, which not only serves as a scaffold but also facilitates cell proliferation, adhesion, migration, and intercellular communication. The extracellular matrix is essential in many aspects of homeostasis, from tissue development to wound healing. Furthermore, abnormalities in its structure and function underlie many cancers and degenerative disorders.
What is the Extracellular Matrix?
The extracellular matrix encompasses a wide range of proteins that provide physical and biochemical support to tissue-resident cells, providing mechanical support and an organized intercellular structure. The components of ECM and cell membrane receptors are in constant communication to inform cellular functions and tissue architecture.
Collagens
Collagen is a fibrous protein that makes up most of the total protein content in mammals. A single collagen protein comprises three polypeptide chains twisted into a triple helix and stabilized by hydrogen bonds.
Elastin
Elastin provides elasticity and resilience for several tissues, allowing them to return to their original shapes after stretching. It is especially abundant in organs and tissues, such as lungs, arteries, and skin, which expand and contract regularly to function. Thus, it contributes to tissue resilience provided by collagen.
Laminin
Laminin is an integral component of the basement membrane, an extracellular matrix layer surrounding epithelial cells. It is a cross-shaped glycoprotein, where the end glycans interact with cell surface receptors and other ECM proteins to glue cells and the ECM together. In addition, it influences cell survival, morphology, migration, and differentiation by interacting with the signal transduction networks.
Fibronectin
Another glycoprotein is fibronectin, which connects cells to the other components of the extracellular matrix. It recognizes the integrins on cell surfaces to mediate cell adhesion. Fibronectin is also found in blood plasma to assist with clot formation and wound healing.
Glycosaminoglycans (GAGs)
Glycosaminoglycans (GAGs) are long linear polysaccharide chains composed of repeating disaccharide units. Because of their negative charges, they can attract water to the tissue. The resulting water retention is a crucial feature of the extracellular matrix, giving it a gel-like structure that provides cushioning against compressive forces. GAGs also control the diffusion of other ECM components and nutrients. A well-known example is hyaluronic acid (HA), which makes up the synovial fluid, providing lubrication for joints to prevent friction during movement.
See how Danaher Life Sciences can help
Functions of the Extracellular Matrix
Structural support for cells and tissues
The extracellular matrix (ECM) provides scaffolding for many cell types, positioning them in 3D space to determine the shape and mechanical properties of the tissue they belong to. Without ECM, bones would not be stiff, and lungs would not be flexible.
Role in cell signaling and communication
The extracellular matrix is in constant communication with cells. ECM components like collagen, fibronectin, and laminin interact with the integrins on cell surfaces to trigger signaling cascades that determine cell behavior. It also provides physical cues for cells, such as stiffness and elasticity, to guide their differentiation and migration.
Regulation of cell behavior and function
Extracellular matrix stores soluble factors, such as growth factors, cytokines, and chemokines, which bind cell receptors to activate cell signaling pathways essential in proliferation, differentiation, migration, and controlled apoptosis.
Contribution to tissue repair and regeneration
The extracellular matrix (ECM) is crucial to tissue remodeling and regeneration upon injury. Collagen and fibronectin in the ECM can bind platelets to promote clot formation. Furthermore, proteoglycans and matrix metalloproteinases in the ECM drive inflammation to remove pathogens and dead cells.
Types of Extracellular Matrix
There are two main types of extracellular matrix. The interstitial (connective tissue) ECM is predominantly found in connective tissue types, including bone, cartilage, tendons, and dermis, forming a fibrous network around the cells. The basement membrane is a specialized type of ECM surrounding epithelial and endothelial tissues that constitute organs and blood vessels. It compartmentalizes special tissues from the connective tissue.
Nevertheless, the composition and function of the extracellular matrix varies depending on the needs of the tissue it encapsulates. While the bone ECM is rich in type I collagen, which is necessary for stiffness, cartilage ECM is enriched in type II collagen and aggrecan for resistance to compression. Another example of specialized forms of the extracellular matrix is the brain ECM, which is lower in fibrous proteins than other ECMs but richer in the proteoglycans of hyaluronan and chondroitin sulfate, which regulate synaptic activity and neuroplasticity.
Extracellular Matrix and Disease
How ECM alterations contribute to diseases
The extracellular matrix is a dynamic environment that can lead to various diseases when dysregulated.
Fibrosis is one of the most severe consequences of ECM malfunctioning. It is caused by the excessive production of collagens, which leads to tissue damage. Fibrosis may manifest in several organs, including the liver (cirrhosis), lungs (pulmonary fibrosis), and kidneys (chronic kidney disease), associated with severe risks of organ failure.
Due to the strong relationship between the extracellular matrix and intracellular signaling pathways, perturbations to the ECM can promote tumor progression. Tumor cells can remodel the extracellular matrix to promote growth and metastasis.
Excessive cytokine storage may attract immune cells to the tissues to promote chronic inflammation. Autoimmune diseases, such as rheumatoid arthritis and multiple sclerosis, are characterized by the degradation of the ECM due to chronic inflammation.
Structural changes to collagen and elastin inevitably occur throughout the lifespan of an individual. As a result, the extracellular matrix becomes stiffer and less elastic, which impairs wound healing and tissue regeneration while increasing the possibility of the diseases mentioned above.
ECM in Biotechnology and Medicine
Applications of ECM in tissue engineering
The composition and structure of the extracellular matrix make it an ideal candidate for regenerative medicine, where it can be used as a blueprint for designing biomaterials for tissue growth and repair. The applications of these biomaterials include synthetic scaffolds for skin and internal organs, hydrogels for wound healing, 3D printing for tissue engineering, and stem cell therapy.
Use of biomaterials derived from ECM in regenerative medicine
ECM components, fibroblasts, and growth factors can be molded into hydrogels, which work in wound healing, cartilage, and spinal cord repair. ECM proteins can also be combined with polymers, such as poly(lactic-co-glycolic) acid (PLGA) and polyethylene glycol (PEG), to produce artificial scaffolds employed in building bone grafts, nerve conduits, and engineered blood vessels.
Research trends
A key challenge in ECM-based biomaterial synthesis is bioactivity and biocompatibility. It particularly poses a challenge in regenerative medicine, as the patient's immune system may reject the scaffold upon detecting foreign cells and proteins.
Decellularized ECM (dECM) is a potential solution to implant rejection. dECM is a type of extracellular matrix harvested from patient tissues, where cellular components are removed, and the key proteins are retained. By incorporating soluble factors from patient tissues, dECMs retain tissue-specific signals to promote desired biological functions.
3D bioprinting is a technology that empowers not only tissue-specific patches and implants but also 3D cell models for drug discovery and research. The combination of ECM components, stem cells, fibroblasts, and growth factors are formulated as bioinks used to print multilayered and biologically relevant tissues that mimic a natural cellular environment. 3D bioprinted scaffolds are widely used in cardiac patches, skin grafts, and corneal scaffolds.
See how Danaher Life Sciences can help
FAQs
How do cytokines interact with the extracellular matrix (ECM)?
Cytokines can bind to ECM components like proteoglycans and glycosaminoglycans, allowing localized storage and controlled release. This helps regulate inflammation, immune responses, and tissue repair.
What role does collagen play in the ECM?
Collagen provides structural support and tensile strength to tissues. It also influences cell adhesion, migration, and differentiation by binding cell surface receptors.
How is the ECM involved in tissue engineering?
The ECM serves as a scaffold that mimics the natural environment for cells, supporting tissue regeneration. Decellularized ECM and ECM-based hydrogels are widely used in engineered tissues.
How does the ECM affect cell behavior?
The ECM influences cell shape, migration, growth, and differentiation through mechanical cues and biochemical interactions with cell surface receptors like integrins.
What role does ECM play in cell signaling and communication?
The ECM modulates cell signaling by presenting growth factors and interacting with receptors to activate pathways that guide development, repair, and homeostasis.
References
- Qi Y, Zhou D, Kessler JL, Qiu R, Yu SM, Li G, et al. Terminal repeats impact collagen triple-helix stability through hydrogen bonding. Chem Sci 2022;13(42):12567-12576.
- Hejran AB, Ashrafi H, Baseer AQ, Sarwari A, Monib AW, Hassand MH, et al. The Importance of Hyaluronic Acid in Biological Systems. EJTAS 2024;2(2):730-743.
- Kandhwal M, Behl T, Singh S, Sharma N, Arora S, Bhatia S, et al. Role of matrix metalloproteinase in wound healing. Am J Transl Res 2022;14(7):4391.
- Ortiz C, Schierwagen R, Schaefer L, Klein S, Trepat X, Trebicka J. Extracellular matrix remodeling in chronic liver disease. Curr Tissue Microenviron Rep 2021;2:41-52.
- Jandl K, Radic N, Zeder K, Kovacs G, Kwapiszewska G. Pulmonary vascular fibrosis in pulmonary hypertension–The role of the extracellular matrix as a therapeutic target. Pharmacol Ther 2023;247:108438.
- Rayego-Mateos S, Campillo S, Rodrigues-Diez RR, Tejera-Muñoz A, Marquez-Exposito L, Goldschmeding R, et al. Interplay between extracellular matrix components and cellular and molecular mechanisms in kidney fibrosis. Clin Sci 2021;135(16):1999-2029.
- Di Martino JS, Nobre AR, Mondal C, Taha I, Farias EF, Fertig EJ, et al. A tumor-derived type III collagen-rich ECM niche regulates tumor cell dormancy. Nat Cancer 2022;3(1):90-107.
- Yuan Z, Li Y, Zhang S, Wang X, Dou H, Yu X, et al. Extracellular matrix remodeling in tumor progression and immune escape: from mechanisms to treatments. Mol Cancer 2023;22(1):48.
- Ghalehbandi S, Yuzugulen J, Pranjol MZI, Pourgholami MH. The role of VEGF in cancer-induced angiogenesis and research progress of drugs targeting VEGF. Eur J Pharmacol 2023;949:175586.
- Simsek H, Klotzsch E. The solid tumor microenvironment—Breaking the barrier for T cells: How the solid tumor microenvironment influences T cells. Bioessays 2022;44(6):2100285.
- Elhaj Mahmoud D, Kaabachi W, Sassi N, Mokhtar A, Ben Ammar L, Rekik S, et al. Expression of extracellular matrix components and cytokine receptors in human fibrocytes during rheumatoid arthritis. Connect Tissue Res 2021;62(6):720-731.
- Ghorbani S, Yong VW. The extracellular matrix as modifier of neuroinflammation and remyelination in multiple sclerosis. Brain 2021;144(7):1958-1973.
- Kelly-Scumpia KM, Archang MM, Purbey PK, Yokota T, Wu R, McCourt J, et al. Modulating the extracellular matrix to treat wound healing defects in Ehlers-Danlos syndrome. Iscience 2024;27(9).
- Indermaur M, Casari D, Kochetkova T, Willie BM, Michler J, Schwiedrzik J, et al. Tensile mechanical properties of dry cortical bone extracellular matrix: a comparison among two osteogenesis imperfecta and one healthy control iliac crest biopsies. J Bone Miner Res 2023;7(12):e10826.
- Selman M, Pardo A. Fibroageing: An ageing pathological feature driven by dysregulated extracellular matrix-cell mechanobiology. Ageing Res Rev 2021;70:101393.
- Kim D-S, Lee J-K, Jung J-W, Baek S-W, Kim JH, Heo Y, et al. Promotion of bone regeneration using bioinspired PLGA/MH/ECM scaffold combined with bioactive PDRN. Materials 2021;14(15):4149.
- Schroeder ME, Rodriguez AG, Speckl KF, Walker CJ, Midekssa FS, Grim JC, et al. Collagen networks within 3D PEG hydrogels support valvular interstitial cell matrix mineralization. Acta Biomater 2021;119:197-210.
- Brown M, Li J, Moraes C, Tabrizian M, Li-Jessen NY. Decellularized extracellular matrix: new promising and challenging biomaterials for regenerative medicine. Biomaterials 2022;289:121786.
- Bejleri D, Robeson MJ, Brown ME, Hunter J, Maxwell JT, Streeter BW, et al. In vivo evaluation of bioprinted cardiac patches composed of cardiac-specific extracellular matrix and progenitor cells in a model of pediatric heart failure. Biomater Sci-UK 2022;10(2):444-456.
- Daikuara LY, Chen X, Yue Z, Skropeta D, Wood FM, Fear MW, et al. 3D bioprinting constructs to facilitate skin regeneration. Adv Funct Mater 2022;32(3):2105080.
- Zhang M, Yang F, Han D, Zhang S-y, Dong Y, Li X, et al. 3D bioprinting of corneal decellularized extracellular matrix: GelMA composite hydrogel for corneal stroma engineering. Int J Bioprinting 2023;9(5):774.
- Heo JH, Kang D, Seo SJ, Jin Y. Engineering the extracellular matrix for organoid culture. Int J Stem Cells 2022;15(1):60-69.
Overview of Extracellular Matrix (ECM)