Steven Henck, PhD, is Vice President of R&D at Integrated DNA Technologies, a global genomics solutions provider helping to accelerate scientific breakthroughs. IDT has developed proprietary technologies for genomics applications such as next generation sequencing, CRISPR genome editing, synthetic biology, digital PCR, and RNA interference. Visitwww.idtdna.com for more information.
One of the most difficult aspects of oncology is the troublesome nature of tumor cells. They are hard to get rid of and can reappear at any time. To make matters worse, their lingering presence after a patient has finished treatment can drastically worsen that patient’s prognosis. In addition to cancer relapse, tumor cells can become resistant to treatment and continue to thrive, leading to disease progression. The impact that surviving tumor cells, or minimal residual disease (MRD), have on patient prognosis makes the ability to detect their continued presence a crucial part of oncology research and therapy.
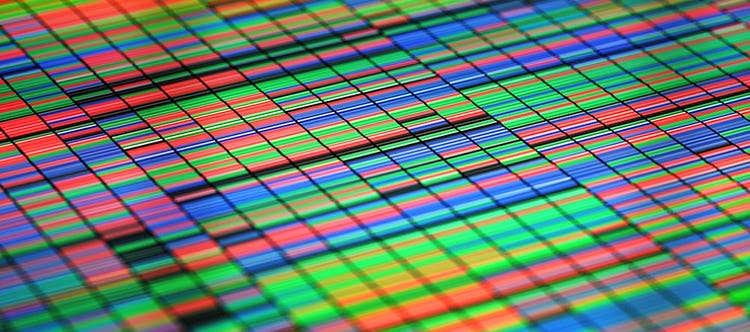
By using a panel that is designed to be personalized for that patient, they are able to optimize the sequencing to detect tumor cells at lower levels. Using panels to target only the genes that are relevant to a patient’s tumor allows for those genes to be sequenced deeply and detected from the small amount of cfDNA in a blood sample. In addition to detecting single nucleotide changes, targeted NGS panels provide more information on other types of tumor markers like methylation or fragmentation patterns, which are becoming more commonly used markers.
"Combined with ever-improving sequencing chemistry, the detection ability of MRD sequencing assays should continue to improve in the coming years "
The Future of MRD Using NGS
To better identify the presence of tumor cells, oncologists are turning to next-generation sequencing (NGS). By sequencing the cell-free DNA (cfDNA) in a patient’s bloodstream, oncologists can detect cancer mutations in DNA shed from cancer cells. The presence of these mutations in cfDNA indicates that tumor cells are present in the patient’s body—and there is a growing body of evidence that cfDNA can be used to find lower levels of MRD than other currently available methods.
Research into the detection of MRD is useful in several different contexts, from potential monitoring of disease progression to opportunities for tracking response to treatment. After a tumor is resected and the patient has undergone treatment, detecting MRD gives clinicians feedback on the effectiveness of the treatment and allows them to tailor care based on the patient’s response. If tumor cells are still detected after treatment, this could suggest that the tumor might be resistant to treatment, thereby signaling the need for clinicians to reevaluate and decide if the patient would benefit from other options. If MRD is not detected, then clinicians can ease off harsh treatments and focus on keeping cancer in remission. After patients have been in remission, MRD detection can be used as a way to track if tumor cells are reemerging and quickly catch a relapse.
Approaches to Detecting MRD
There are two different ways that NGS is currently being used to detect MRD, depending on the information available to clinicians. When clinicians do not know which specific mutations are found in a tumor, they can sequence the cfDNA using a panel of universal cancer markers to detect the presence of MRD in a tumor-naïve approach. When clinicians have sequenced a tumor and know the mutations that it contains, they are able to take a tumor-informed approach and select a panel of markers that are specific for the mutations related to that patient’s unique cancer cells.
Using NGS to detect MRD is not without its own challenges. The nature of sequencing cfDNA to detect markers from a small number of tumor cells means that there will be a limited number of these marker sequences present in the sample. This makes detection difficult and sensitivity even more paramount. Library preparation must be very efficient so that as many possible fragments of tumor-derived DNA actually make it onto the sequencer. The requirement for high sensitivity also underscores the need for panels that target these markers evenly to allow for deep sequencing in a cost-efficient manner. It also demonstrates the need for the best possible markers for these panels, which are currently being improved through research efforts. Combined with ever-improving sequencing chemistry, the detection ability of MRD sequencing assays should continue to improve in the coming years. These assays also face the challenges that are inherent to all potential diagnostic tests. Large-scale clinical trials are still needed to demonstrate the clinical utility of detecting MRD using NGS, and being able to minimize turnaround time and cost will continue to be key focus areas. To successfully implement these assays, being able to quickly design panels, sequence a patient’s circulating cfDNA, and analyze the data will be important.
Using NGS to detect MRD has the power to improve our ability to detect tumor cells after a patient has undergone treatment. By utilizing panels of tumor markers that can be customized for a patient’s specific tumor, cfDNA can be sequenced with the sensitivity needed to detect small amounts of tumor DNA in a blood sample. This allows clinicians to non-invasively track disease progression and monitor relapse using a quickly developing method that has shown the ability to outperform current detection approaches. This makes MRD detection using NGS an exciting emerging technology that will alert clinicians to MRD sooner, leading to faster responses and—and hopefully— improved patient outcomes.
This article by one of our Danaher Life Sciences thought leaders was originally published in Life Sciences Review. Shared here by permission.
Improving Minimal Residual Disease Detection Using NGS